We recommend RSV Vaccine for pregnancy 32-36 weeks between September and January.
We recommend the Pfizer RSV vaccine if you are 32 to 36 weeks pregnant from September to January. The vaccine creates antibodies that pass to your fetus. This means the baby will have some antibodies to protect them from RSV for the first 6 months after birth.
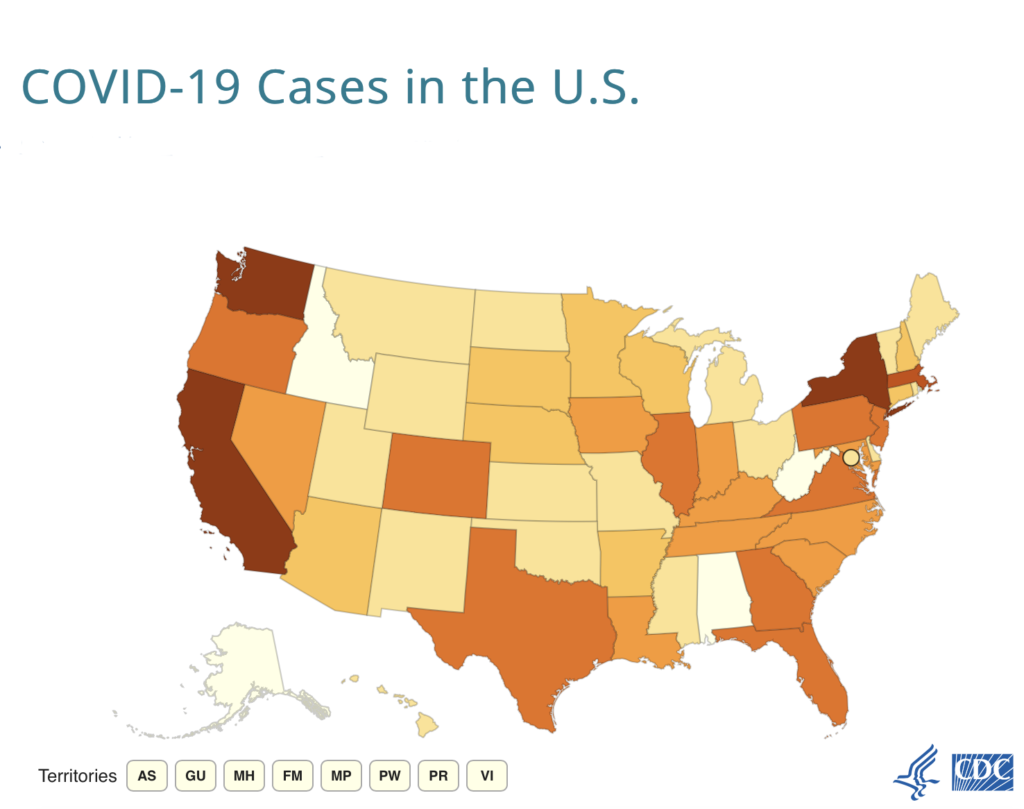
RSV, or respiratory syncytial virus, is a virus that spreads in the fall and winter. RSV can be dangerous for babies and young children. It is the leading cause of hospitalization among infants in the United States.
There are multiple RSV vaccines approved by the U.S. Food and Drug Administration (FDA). The only RSV vaccine approved by the FDA for use in pregnancy is the one made by Pfizer. It is called Abrysvo.
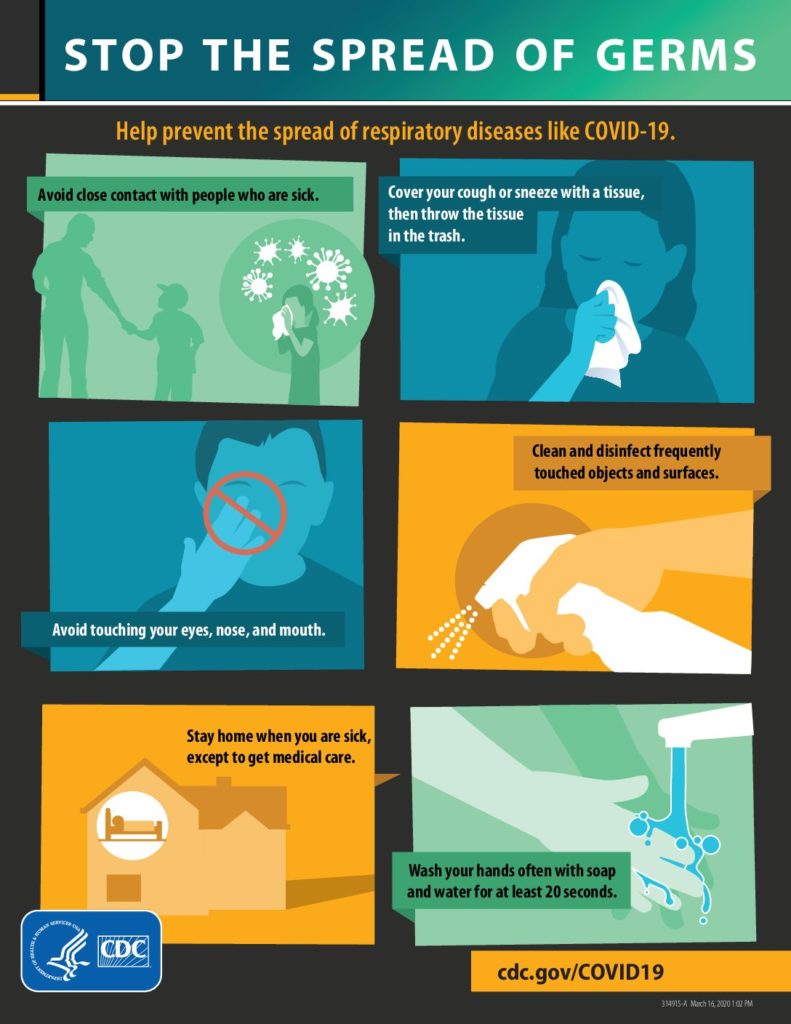
You can get the Pfizer RSV vaccine at the same time as other vaccines recommended during pregnancy. Common side effects of the RSV vaccine include arm pain, headache, muscle pain, and nausea, similar to other vaccine side effects. Side effects are normal and not a cause for concern.
The RSV vaccine is one of two new options for protecting babies during RSV season. There is also an option to give babies an injection called Nirsevimab. Nirsevimab contains lab-made antibodies that protect against RSV. It is not a vaccine. Please talk to your pediatrician to see if this is an option at their office for your newborn.
You can get the Pfizer RSV vaccine at the same time as other vaccines recommended during pregnancy.
In most cases, you should choose between the RSV vaccine during pregnancy and Nirsevimab after birth. The goal is to protect your baby from RSV, either with antibodies made during pregnancy or with antibodies given directly to your baby after birth.
We can help you decide between these two options. You may want to consider the following:
The RSV vaccine gives your baby protection right after birth. If you get the RSV vaccine, there is one less injection for your baby to get after birth. Nirsevimab may provide your baby with longer-lasting protection but confirm with your pediatrician, this will be an option for your baby at their office. It may be hard to get Nirsevimab this fall and winter.
• • •
List of pharmacies our pregnant patients have received their vaccines without issue:
- Walmart in Germantown
- Costco in Gaithersburg