The field of medicine is changing rapidly through the advances made by genomic technology. We are on the verge of an exciting era where we will be able to have personalized medical care and treat each person based on his or her individual risks. For example, every woman fits into one of three risk categories for breast cancer. A person may face only a sporadic risk with the same risk as the general population, or their risk may be increased due to a positive family history, or increased even more if they are discovered to have an inherited genetic risk. Focusing on a person’s family history gives us the opportunity to detect those people who face a significantly increased danger of developing cancer and then use proven successful strategies to reduce that risk.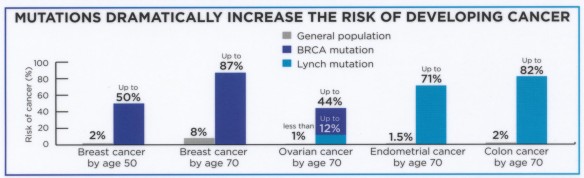
Cancer screening depends on risk. Women who face only the sporadic risk of breast cancer do not need additional screening beyond that for the general population: regular mammography starting at age 40. Those who have an increased risk due to family history or who have dense breasts would benefit from more frequent screening with mammography, breast ultrasound or breast magnetic resonance imaging starting at least 10 years prior to the age of cancer diagnosed in their youngest affected relative. A small number of women carry the highest risk for gynecologic cancer due to having a defective gene. BRCA gene carriers, for example, should have testing started 15 years earlier than average, and usually benefit from oral contraceptives to decrease the risk of ovarian cancer. They also benefit from surgery to reduce their risk such as preventative removal of the ovaries, as otherwise the risk of ovarian cancer can be as high as 44% by age 70.
There are about 1 million people in the United States carrying genes for the most common hereditary gynecologic cancers: BRCA and Lynch syndrome. Hereditary Breast and Ovarian Cancer syndrome (HBOC) is seen in approximately 10% of breast and ovarian cancer patients. This autosomal dominant genetic disorder is caused by mutations in tumor suppressor genes BRCA1 and BRCA2. Red flags for HBOC syndrome include a three generation family history positive for breast cancer prior to age 50, bilateral, triple negative or male breast cancer, ovarian cancer at any age, prostate, pancreatic or melanoma cancer under age 50, Ashkenazi Jewish population, or a known BRCA mutation in the family.
About 20% of colon and endometrial cancers are associated with a strong family history of cancer. 5% occur in autosomal dominant genetically defined high-risk syndromes such as Lynch syndrome. Risk factors for Lynch syndrome include colorectal or endometrial cancer before age 50, colorectal cancer in 2 generations on the same side of the family, ovarian or gastric cancer at any age, and 2 or more individuals with colon, endometrial, ovarian, gastric, brain, biliary, pancreatic, or small bowel cancers.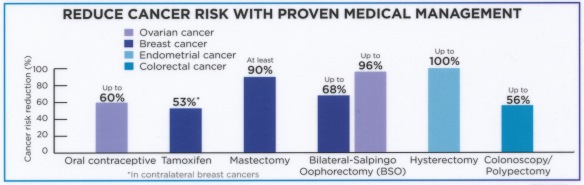
Cancer risk assessment is one of the key parts of the annual well woman exam. Standard pap testing has been successful in reducing cervical cancer, and so too can screening for hereditary cancers result in cancer prevention and early detection. Knowing one’s cancer risk can guide lifestyle choices and the choice of medications that can safely decrease cancer risk. 10% of people carry increased cancer risk, and approximately 6% of people have increased genetic family risk that makes them eligible for testing to determine if their risk is greatly higher than was previously thought. If positive, this result can have a positive impact on not only the patient, but also their relatives and their descendants.
With our understanding of cancer genetics progressing rapidly, knowing one’s detailed family history and then determining who is at increased cancer risk can be of great value in having a safer, healthier life.
