Pregnancy is a great time, an exciting time, but it’s also a time of endless questions. Women have access through social media, television, print media, Internet searches, and their friends to much information about pregnancy, but sometimes it can be confusing or wrong. There are many questions about all facets of life including eating, drinking, sleeping, working, travel, exercise and having sex. We are often asked these questions by our patients, and in the recent issue of our professional publication, Obstetrics and Gynecology (April 2018, p713), Dr. Fox wrote a nice summary about current, science-based recommendations regarding these topics. I’m going to summarize them for you in this article.
Prenatal Vitamins
Prenatal vitamins are designed to meet the needs of pregnant women. However, except for folic acid, iron and Vitamin D, it’s unknown if taking them makes a difference in outcome. For women with well-balanced nutritious diets, they are probably not required. Folic acid deficiency is associated with fetal birth defects, so women who don’t have it in their diet should be on 400-800 micrograms a day. Women who have had a history of a previous pregnancy complicated with a neural tube defect should be on 4,000 micrograms a day. Iron supplementation is advised to increase the mother’s blood count to avoid becoming anemic at birth. It is more needed if the mother’s blood count is low to begin with. Vitamin D deficiency is associated with pregnancy problems including pre-eclampsia and premature birth. While testing for Vitamin D levels is not routinely recommended, taking Vitamin D (usually 200-600 IUs) daily is. Calcium supplementation has been shown to decrease high blood pressure in pregnancy. Women should be sure to consume through diet or supplements at least 1,000 mg of calcium per day. Some prenatal vitamins don’t have that much.
Nutrition and Weight Gain
Pregnant women should eat a healthy, well-balanced diet and usually should increase their calorie intake in the second and third trimesters by only a small amount, about 350-450 calories per day. A good nutrition resource is a website run by the U.S. Department of Agriculture at www.chooosemyplate.gov. Women with higher pre-pregnancy weight should not gain as much as women with normal or low weight.
Alcohol
High alcohol intake in pregnancy has been associated with fetal malformations. Studies in Denmark and Australia have found no association between a low level of maternal drinking (less than one drink per day) and developmental cognitive abilities in children. However, the threshold for safe drinking is not known, and it can’t be concluded that a small amount of drinking is safe. All major health organizations recommend abstaining from alcohol completely during pregnancy.
Artificial Sweeteners
There is no evidence that aspartame (NutraSweet), sucralose (Splenda), acesulfame potassium (Sunett), stevioside (Stevia) or saccharin (Sweet N Low) cause birth defects.
Caffeine
Most studies in humans show that low to moderate caffeine use is not associated with any adverse outcomes. Some animal studies suggest that high caffeine intake (greater than 10 cups per day) slightly increases the risk of miscarriage.
Fish
Eating fish conveys both benefits and potential risks. Benefits are that studies have shown eating fish in pregnancy resulted in improved neurodevelopment in children, and also lowered the risk of premature birth. However, fish is also a potential source of mercury exposure and mercury can cause harm. Therefore pregnant women should try to consume 2 to 3 portions weekly of fish that are high in long chain polyunsaturated fatty acids and low in mercury, such as anchovies, Atlantic herring, Atlantic mackerel, mussels, oysters, farmed and wild salmon, sardines, snapper, and trout. Other safe fish which have less fatty acids include shrimp, pollock, tilapia, cod and catfish. Women should avoid fish with higher mercury content such as king mackerel, shark, swordfish, marlin, and tilefish. For women who do not consume 2 to 3 servings of fish a week, there is no clear evidence that supplementation with omega-3 fatty acids improves outcome in children, but they are unlikely to be harmful.
Most health organizations advise women to avoid raw fish in pregnancy. However, the fish that typically makes up sushi (tuna, salmon, yellow tail, snapper, flounder) rarely carries parasites. Therefore, the risk of infection from eating well-prepared sushi in a clean and reputable establishment is not significant.
Other Foods to Avoid
Food restrictions in pregnancy are designed to minimize exposure to harmful infections such as toxoplasmosis and Listeria. To lower the risk of toxoplasmosis, avoid eating raw and undercooked meat, and wash all fruits and vegetables before eating them. To lower the risk of Listeria, avoid unpasteurized dairy products, raw sprouts, unwashed vegetables, and unheated deli meats. While Listeria outbreaks were linked to deli meats in the 1990s, recently outbreaks were caused by ice cream, cantaloupes, hummus, and unpasteurized dairy products, so it’s difficult to make a list of safe foods without becoming overly restrictive.
Smoking and Nicotine
Smoking in pregnancy is harmful to both maternal health and to fetal health, causing many possible pregnancy complications. Although some of the adverse effects of smoking are due to nicotine, nicotine products designed to aid in smoking cessation are acceptable as part of a smoking cessation program, since nicotine in gum or a patch would reduce exposure to other toxins in cigarettes and in second hand smoke. Other interventions such as bupropion and varenicline are thought to be effective and safe, but data is limited. Electronic nicotine delivery systems such as electronic cigarettes and vaporizers deliver high amounts of nicotine and could potentially be harmful, but less is known about them.
Marijuana
Marijuana is the most common illicit substance used in pregnancy. Current evidence shows that marijuana use in pregnancy is not associated with premature birth, low birth weight, or an increased risk of birth defects. Doses of it are not regulated and could vary significantly. Current recommendations are to avoid marijuana in pregnancy due to concerns about fetal neurodevelopment.
Exercise and Bedrest
Women with normal pregnancies should engage in regular aerobic and strength conditioning exercise. It is prudent to avoid exercise with a higher risk of injury such as contact sports, downhill skiing, and horseback riding. Women should try to moderately exercise 20-30 minutes four to five times a week. Moderate exercise is at the level at which women can still talk while exercising.
Bedrest, or activity restriction, is associated with several risks and has not been shown to be beneficial in pregnancy. Activity restriction has not been shown to be beneficial for women with high blood pressure, premature rupture of membranes, fetal growth restriction, or placenta previa.
Avoiding Injury in the Car
Pregnant women should continue to use three-point seatbelts in pregnancy. The lap belt should be placed across the hips and below the uterus. While airbags can also reduce the risk of injury, deployment of an airbag itself can also cause injury. It’s unclear if they are beneficial or harmful.
Oral Health
Oral health and routine dental procedures should continue as scheduled during pregnancy, including cleanings, extraction, root canal and fillings. X-rays can be done if the abdomen and thyroid are shielded.
Hot Tubs and Swimming
Hot tubs have the potential to increase body temperature, which is considered a risk for miscarriage and birth defects. It is thought to be more potentially harmful if it is done within the first 4 weeks from the last menstrual period, or if it is done more often.
Swimming pools are typically maintained below normal body temperature, and their use is not associated with harmful outcomes.
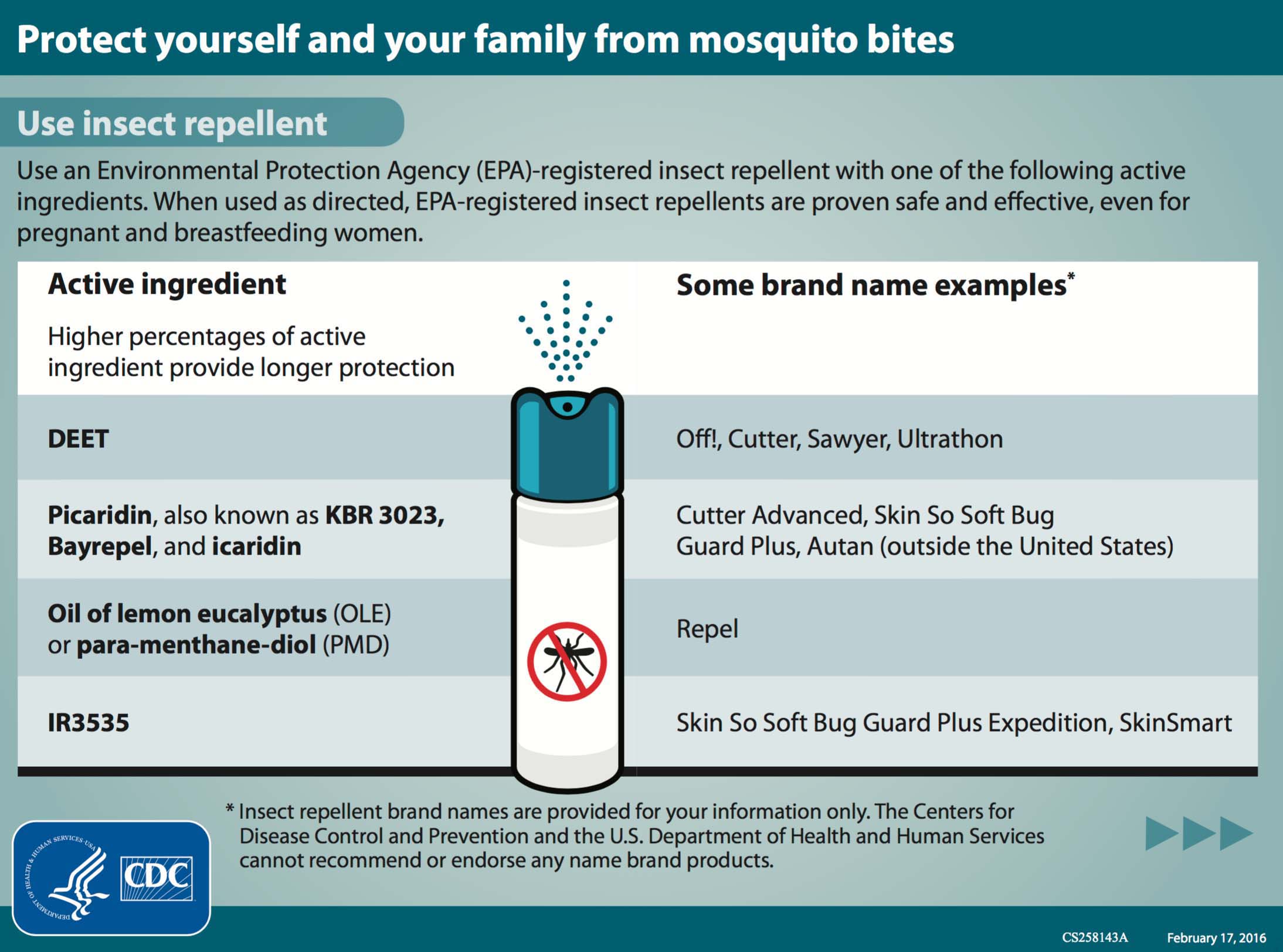
Insect Repellents
Topical insect repellants can be used in pregnancy because they are not associated with adverse fetal effects. As a result of the risk of mosquito-borne illnesses including Zika virus, their use in high risk areas is recommended.
Hair Dyes
Most studies on exposure to hair dye relate to the profession of cosmetology, and studies are mixed as to whether or not there is increased risk of pregnancy loss in that setting. Data on safety is limited, but for an individual pregnant woman, exposure to hair dye results in minimal systemic absorption, so hair dyes are presumed safe in pregnancy.
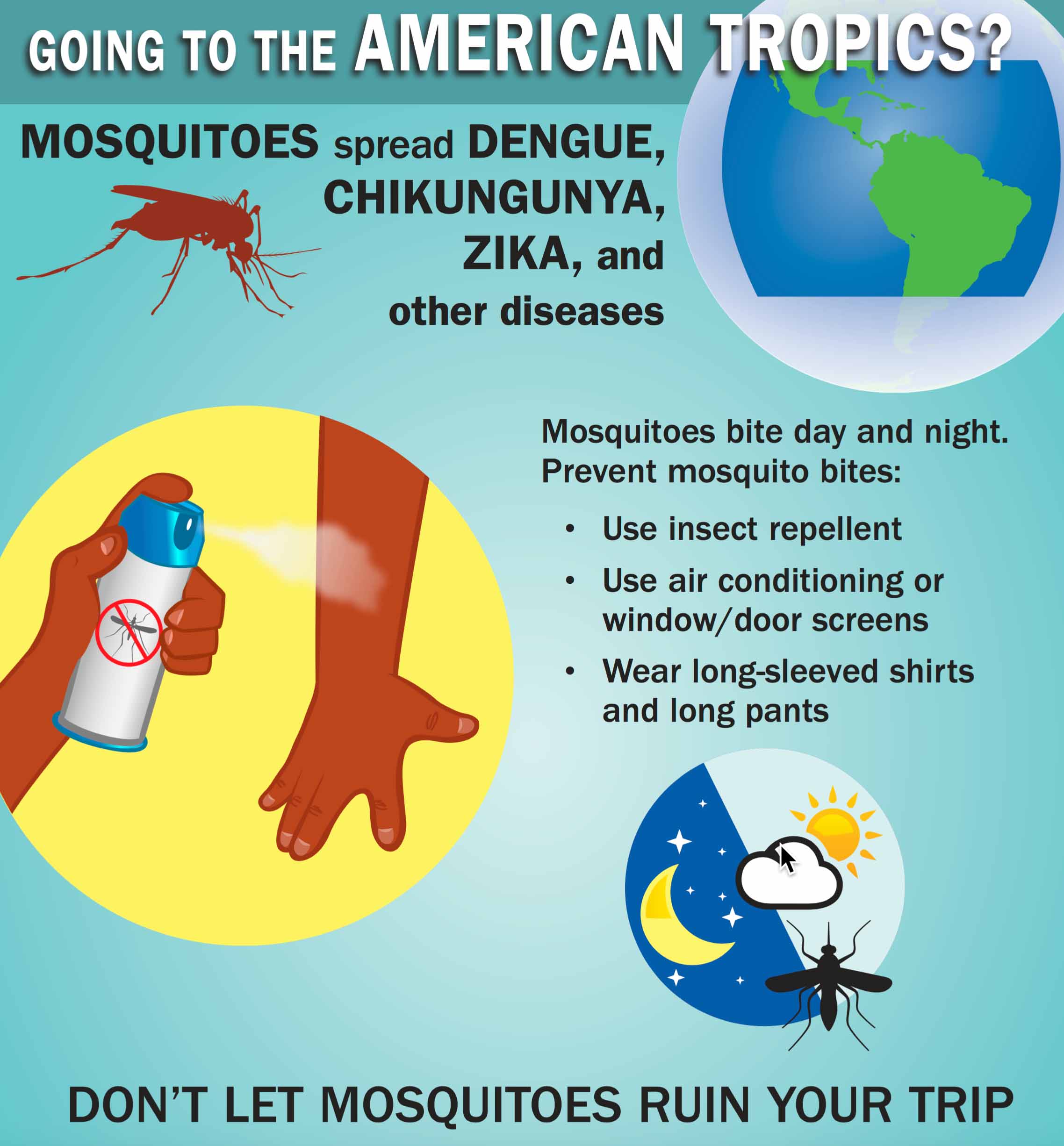
Travel
Airline travel is considered safe in pregnancy, but it is prudent to take precautions to lower the risk of a blood clot by periodic walking. Pregnant women may go through security metal detectors. The radiation exposure from the newer backscatter units is also safe. In regard to travel destinations, women should be aware of the potential infection exposures (including Zika virus) as well as the availability of medical care at their destination. As the length of the pregnancy advances, the risk of travel increases, but there is no exact gestational age at which women cannot travel. In our office, it’s our policy to not allow distant travel in the last two months.
Sexual Intercourse
Sex and orgasm are not associated with an increased risk of pregnancy complications or premature birth. For women with vaginal bleeding or ruptured membranes, the risks of bleeding or infection may increase. Although there is little data to support it, most authorities recommend avoiding sexual intercourse after 20 weeks of pregnancy if a placenta previa is present.
Sleeping Position
Women are frequently advised to sleep on their sides, especially the left side. Several retrospective studies (limited by recall bias) have shown an increased risk of stillbirth when sleeping flat on one’s back. Considering the limitations of these studies as well as not knowing more about the benefits of side sleeping, it’s unclear if side sleeping conveys a benefit, how much it reduces risk and when. It’s our recommendation to not sleep flat on your back in the last 2 months of pregnancy. Sleeping on your side or on your back being tilted up by additional pillows should be safe.






 Once a person is infected, the incubation period for the virus is approximately 3-12 days. Symptoms of the disease are non-specific but may include fever, rash, aching in joints, and eye inflammation. It appears that only about 1 in 5 infected people will have these symptoms and most will have mild symptoms. It is not known if pregnant women are at greater risk of infection than non-pregnant.
Once a person is infected, the incubation period for the virus is approximately 3-12 days. Symptoms of the disease are non-specific but may include fever, rash, aching in joints, and eye inflammation. It appears that only about 1 in 5 infected people will have these symptoms and most will have mild symptoms. It is not known if pregnant women are at greater risk of infection than non-pregnant. has been associated with birth defects, specifically significant microcephaly (small fetal head). Transmission of Zika to the fetus has been documented in all trimesters; Zika virus RNA has been detected in fetal tissue from early miscarriages, amniotic fluid, babies and the placenta. However, much is not yet known about Zika virus in pregnancy. Uncertainties include the incidence of Zika virus infection among pregnant women in areas of Zika virus transmission, the rate of transmission to the fetus, and the rate with which infected fetuses have complications such as microcephaly or demise. The absence of this important information makes management in the setting of potential Zika virus exposure (i.e. travel to active areas) or maternal infection, difficult. Currently, there is no vaccine or treatment for this infection.
has been associated with birth defects, specifically significant microcephaly (small fetal head). Transmission of Zika to the fetus has been documented in all trimesters; Zika virus RNA has been detected in fetal tissue from early miscarriages, amniotic fluid, babies and the placenta. However, much is not yet known about Zika virus in pregnancy. Uncertainties include the incidence of Zika virus infection among pregnant women in areas of Zika virus transmission, the rate of transmission to the fetus, and the rate with which infected fetuses have complications such as microcephaly or demise. The absence of this important information makes management in the setting of potential Zika virus exposure (i.e. travel to active areas) or maternal infection, difficult. Currently, there is no vaccine or treatment for this infection.